Families come in all shapes and sizes, and the path to parenthood isn’t always as straightforward for some individuals as it is for others. But those who face detours along the way still have options, and even though the road may appear to be closed at one point, it doesn’t have to be permanently so.
More than half a million men in the U.S. get a vasectomy each year, and of that group, approximately 12% end up regretting the decision later on. The most common reason is a change in their relationship status—perhaps they got divorced and hope to have a child with their new partner—or they may have lost a child or simply had a change of heart.
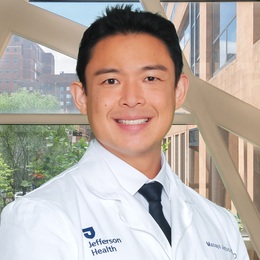
No matter what the motivation, a vasectomy reversal is a safe and effective surgical procedure that has great success rates in restoring fertility and allowing men to once again start a family or expand their existing one. Jefferson Health has become one of the leaders in the region for this procedure under the direction of Masaya Jimbo, MD, PhD, a highly skilled urologic microsurgeon.
“No matter how recent or how far in the past you had the vasectomy, I would consider you a good candidate for a vasectomy reversal,” Dr. Jimbo says. “Now, some studies have shown that if you are much more than 20 years out from having your vasectomy, there is increased risk of the surgeon needing to perform a complex repair, as opposed to a simple repair during the vasectomy reversal. That is associated with less likelihood of success in terms of sperm coming back to the ejaculate. But everybody is a candidate and there are certainly men who are decades out from having a vasectomy where we can perform a simple connection and we can expect good results.”
Female factor fertility also plays a role, and in cases where in vitro fertilization (IVF) is highly recommended or necessary for the woman, a vasectomy reversal may not be the best option, Dr. Jimbo explains, because natural conception would be difficult for such couples. In those instances, he suggests a testicular sperm extraction, which is where sperm is retrieved directly from the man’s testicles and can be used for assisted reproductive techniques such as IVF.
But when the situation does call for a vasectomy reversal, Dr. Jimbo has undergone the specialized training and provides the meticulous attention to detail required for the surgery, leading to success rates exceeding 90% in many cases. At Jefferson Health, he also has the advantage of state-of-the-art technology, including a high-powered microscope known as an ORBEYE.
“A vasectomy is a very straightforward procedure, and any urologist who did a standard urology residency should be qualified to do it,” he explains. “It takes 15 to 20 minutes in the office and the patient is usually awake, and all we need are numbing medications. A vasectomy reversal is a completely different animal.
“It can take, depending on the anatomy of the patient and the skill of the surgeon, anywhere between two and a half to five hours, and it requires subspecialty fellowship training in microsurgery that you cannot get from a standard urology residency.”
A vasectomy reversal reconnects the severed ends of the vas deferens—the tubes that carry sperm from the testicles—that were “snipped” during the vasectomy. Depending on the amount of scar tissue that has to be removed and the presence of sperm in the vas, either a simple connection—a vasovasostomy—or a complex connection—a vasoepididymostomy—is then performed. The former has success rates between 90-95%, while the latter takes longer but still has success rates of around 60-80%.
Both types of surgery have the same recovery time, and Dr. Jimbo advises patients to take things easy for at least four weeks, and up to eight weeks if possible.
“We are using sutures that are thinner than your hair to hook things together,” he says. “One pound of force is enough to tear the sutures apart, so you really want to try to minimize your activity or lifting for a long period of time to make sure you don’t accidentally tear apart the sutures.”
Dr. Jimbo praises Jefferson Health for establishing a protocol in which he has set times to meet with patients interested in a vasectomy reversal so they don’t have to wait months for a consultation and can get the process started. Since June is Men’s Health Month, he also encourages men to stay current with screening for prostate cancer, and to not be embarrassed about seeking help for erectile dysfunction, since it is a common problem for males over 50.
Whatever issue they care concerned about, patients can expect a warm and inviting atmosphere at Jefferson Health.
“Everyone at Jefferson has been extremely supportive in bringing me aboard and doing all they can to kick start this male infertility program, and specifically the vasectomy reversal program,” Dr. Jimbo says. “That support extends to our care of the patients as well. … Once the patient comes to see me, they have 45 minutes to an hour to talk about the vasectomy reversal rather than the standard 15-30-minute slot that you typically get for other types of appointments. We also have a very good finance team and an OR team to take care of you the rest of the way.”
Jefferson Health
Multiple locations in South Jersey
JeffersonHealth.org
Click here to subscribe to the free digital editions of South Jersey Magazine
To read the digital edition of South Jersey Magazine, click here.
Published and copyrighted in South Jersey Magazine, Volume 22, Issue 3 (June 2025)
For more info on South Jersey Magazine, click here.
To subscribe to South Jersey Magazine, click here.
To advertise in South Jersey Magazine, click her