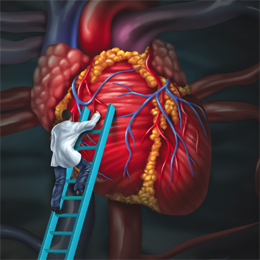
The more you know about heart attacks and strokes, the better your chance at survival. That’s because time is of critical importance when it comes to receiving life-saving treatment. Being able to recognize warning signs early on in yourself—or someone else—can be a matter of life or death.
While everyone is different, according to the American Heart Association, some of the early warning signs of a heart attack include an uncomfortable pressure or pain in the chest, shortness of breath (with or without chest pain) or a pain in the arm (typically the left arm). Women may experience these same symptoms but also may be more likely than men to experience some other lesser known symptoms such as nausea or vomiting or back or jaw pain. Basically, the onset of any symptom that is out of the usual for you should not be ignored.
With a stroke, some of the warning signs include weakness or numbness in an extremity, visual abnormalities, a sudden or severe headache, difficulty speaking, balance problems or slurring of the speech, says Dr. Kenneth Wu, medical director at Kessler Institute for Rehabilitation-Marlton. Unfortunately, Wu says some of these symptoms are easily ignored as a patient simply doesn’t recognize what’s happening. He believes that, likely due to the excellent job the American Heart Association has done, more people are educated on heart attack symptoms than they are stroke ones. That’s likely helped improve the possibility of survival—and he’d like to see stroke education get to that point.
“When patients have a pain in their chest they don’t mess around—they get to the hospital,” Wu says. “I’d like to see this type of reaction with a stroke because as soon as you get care, the better your outcome will be. Time is so important with a stroke.”
Wu says that also means seeing a doctor even if the symptom goes away. That’s another common reason he says some of his patients wait too long to be checked out. They may have had some weakness in their extremity but it disappeared so they assume they’re fine. But Wu says that’s still a reason to be seen by a doctor.
?“Sometimes a symptom that develops but then goes away is because the patient suffered a transient ischemic attack, a ‘mini stroke,’” Wu says. “Five percent of the patients who suffer a TIA will develop a stroke within a month—even if all their symptoms went away.”
Nina Geier, MS, MPT, CBIST, senior director of Bancroft NeuroRehab, says that a memorable way to remember the warning signs of a stroke is to use the acronym FAST, which stands for facial drooping, arm weakness, speech changes, and time to get to the hospital. She advises that patients call 911 at the first sign of one of these symptoms.
Knowing your risk
Though education has improved, heart disease remains the leading cause of death in the United States. Stroke is the third leading cause. Fortunately, there are some risks that can be addressed with both.
“To reduce one’s risk of a heart attack or stroke, we recommend that everyone follow heart healthy lifestyle habits, including regular aerobic exercise and a diet emphasizing vegetables,” says Dr. Douglas Jacoby, medical director, Center for Preventative Cardiology and Lipid Management at Penn Medicine. “Maintaining a normal body weight, avoiding excess alcohol and not smoking are also important components of staying healthy.”
Beyond lifestyle choices, some people have genetic risk that runs in their family. Many people, due to lifestyle or family risk, will benefit from medications to reduce their future risk of a heart attack or stroke.
“These medications may target blood pressure, cholesterol or diabetes,” Jacoby says. “A number of guidelines, including those by the American College of Cardiology and the National Lipid Association, help guide providers and patients to understand who will benefit from medications.”
Paying attention to some of these potential risk factors as well as personal medical problems is critical when it comes to preventative care, agrees Geier.
“Medical factors that increase a person’s risks for heart attacks and stroke include high blood pressure, diabetes, high cholesterol, circulatory problems, atrial fibrillation and lifestyle factors,” Geier says. “It is important to know your personal risk factors and talk with your doctor about how to manage them. An ounce of prevention is worth a pound of care.”
And the future of prevention may hold even more hope as medicine continues to advance. Jacoby says that in the field of preventative cardiology, there has been ongoing progress toward evaluating patients’ future risk, which he says is making doctors more effective at preventing heart attacks and strokes in the first place.
“The younger we start encouraging people to understand their risk and modify their cardiac risk factors, the larger impact we can have in tackling our country’s No. 1 killer,” Jacoby says. “Some of the advances over the last decade include the ability to more accurately individualize care to decide who is truly at risk for a heart attack or stroke, and target these individuals with more intense treatment to lower their risk. By imaging one’s heart with a CT scan and the neck arteries with specialized ultrasound testing, we can identify whether an individual actually has plaque in one’s arteries. In addition, checking advanced blood work enables us to refine our understanding of an individual patient’s metabolic control. This helps us adjust a patient’s treatment goal, determine if he/she benefits from medication and dose medication to optimize risk reduction.”
Advances in rehabilitation
As the medical field has advanced over the years, so have the options for stroke and heart patients. According to Karen Lindgren, Ph.D., senior director of neuropsychology services with Bancroft NeuroRehab Clinical Team, new American Heart Association/American Stroke Association Stroke Guidelines were published in June 2016 for providing post-stroke rehabilitation.
“Of course, initial recovery from stroke requires coordinated medical care in an acute care hospital to establish medical stability,” Lindgren says. “Stroke patients often progress from the acute care hospital to inpatient rehabilitation and then outpatient rehabilitation, which is what we do at Bancroft NeuroRehab, to address post-stroke challenges in physical functioning, communication, cognition and daily living.”
But regardless of the stage of recovery, Lindgren emphasizes that a coordinated team approach is crucial and should include the patient, family/friends, physicians, physical therapists, occupational therapists, speech language pathologists, psychologists, nurses and recreation therapists, among others.
“For ongoing rehabilitation, I recommend stroke patients seek treatment by a team of clinicians with specialized expertise in stroke and neurological conditions,” Lindgren adds. “That’s something that sets Bancroft NeuroRehab apart—we are solely focused on neurological rehabilitation. Each member of a care team needs to focus on the same goals; supporting the patient as he or she reaches full rehabilitation potential and returns to meaningful, productive activities at home, in the community or at work.”
As people become more educated on both heart attacks and strokes, they are seeking care sooner and therefore improving their odds.
“My big take home message for people is to pay attention to their symptoms and don’t ignore them,” Wu sums up. “Don’t just assume something will go away and waste valuable time. Time is the most important factor in your survival and recovery.”
Published (and copyrighted) in South Jersey Magazine, Volume 13, Issue 11 (February, 2017).
For more info on South Jersey Magazine, click here.
To subscribe to South Jersey Magazine, click here.
To advertise in South Jersey Magazine, click here.